An Epidemic Within a Pandemic: The Opioid Crisis and COVID-19
The COVID-19 pandemic has taken priority over nearly all other health crises. However, the opioid epidemic has raged on, concurrent with (and accelerated by) SARS-CoV-2. Despite a 44% decrease in the number of opioids prescribed over the past decade, drug overdose deaths have continued to rise. The most recent CDC data estimate more than 100,000 people a year in America are dying of drug overdose; 3 out of 4 of those deaths are attributed to opioids. The same data show that for the 12-month period beginning in March 2020 — when pandemic shutdowns began in the U.S. — drug overdose deaths from opioids rose 38%. Together, these statistics demonstrate the devastating impact of the COVID-19 pandemic on the opioid crisis.
Even before the COVID-19 pandemic began, certain communities, populations, and regions were more greatly affected by the opioid epidemic than others. A study from the Department of Health and Human Services (HHS) shows how impoverished communities in rural areas in the U.S. have been most impacted, especially those in the south.
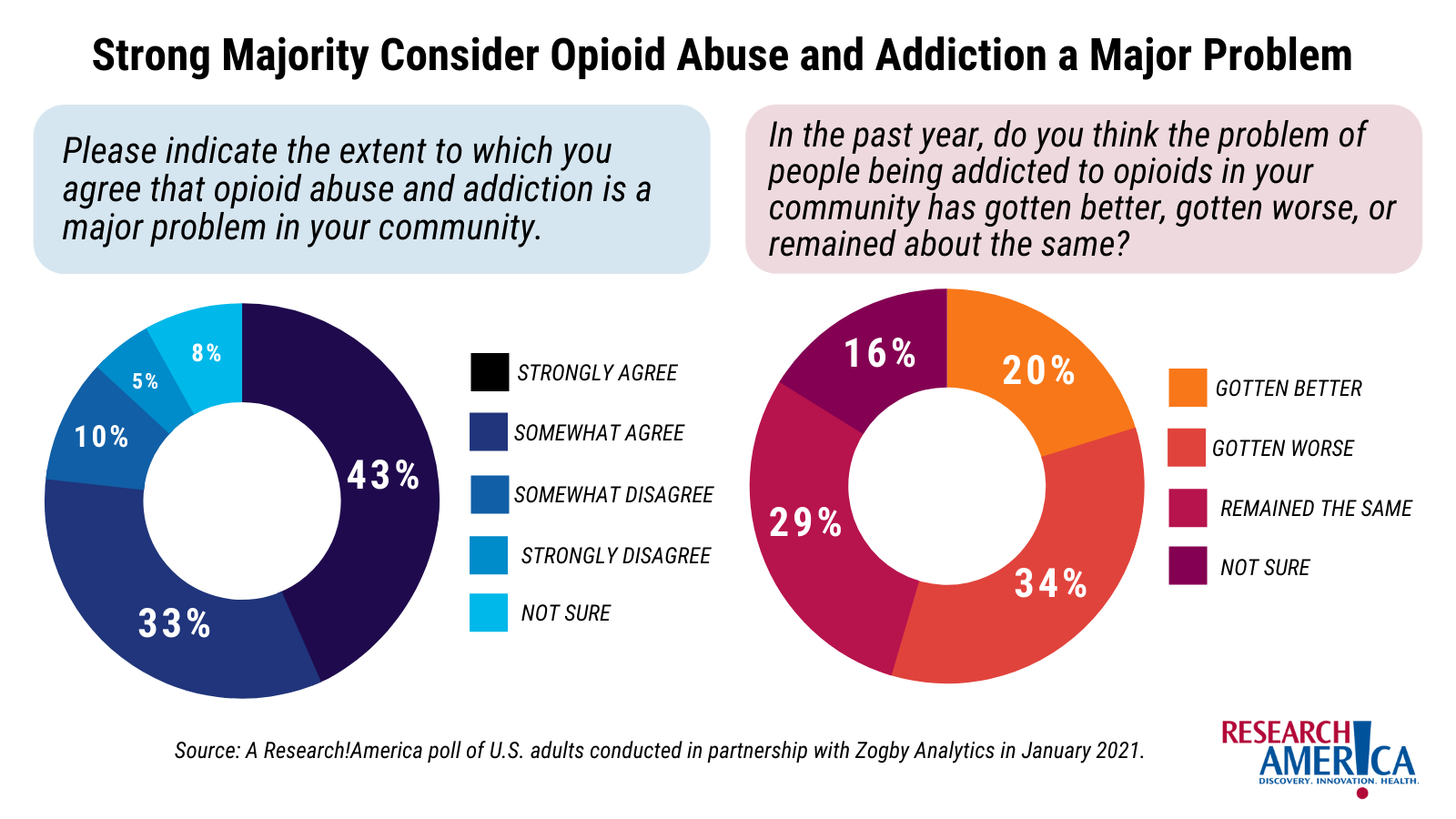
In a 2021 survey commissioned by Research!America, 76% of respondents said they “strongly” or “somewhat” agree when asked if they felt opioid abuse and addiction were a major problem in their community.

Additionally, 63% of respondents said that the problem of opioids in their communities had remained the same or gotten worse, while just 20% said the problem was improving.
Challenges Presented by COVID-19
COVID-19 exacerbated many factors fueling the current opioid crisis. Social isolation and stay-at-home orders can cause loneliness, stress, depression, and anxiety, which are particularly challenging to individuals at risk of developing an addiction,currently experiencing addiction, or in recovery. Early in the pandemic, CNN reported that some patients with opioid use disorder (OUD) who sought treatment didn’t feel safe in residential facilities or in-person treatment programs, due to the risk of contracting COVID-19, but simultaneously watched their support networks fall apart. Obtaining naloxone, a life-saving medication used to reverse opioid overdose, may have also been impacted by COVID-19. A September 2021 report by the American Medical Association mentioned a 26% decrease in the number of naloxone prescriptions filled in retail pharmacies during the COVID-19 pandemic.
Access to treatment has been a challenge in the U.S. for years. According to a Surgeon General’s report from 2016, only 1 in 10 patients with a substance use disorder get the treatment they need. The pandemic made treatment even harder to access for many, according to Dr. Nora Volkow, director of the National Institute on Drug Abuse. Emergency rooms have reduced access and in-person programs, limiting resources like syringe exchange programs and mentoring opportunities.
Fortunately, telemedicine has provided a “major breakthrough,” according to Volkow, in providers’ abilities to reach patients. Physicians can now prescribe medications for OUD without the need to see a patient in person. The CNN report noted how virtual meetings and video calls have allowed providers to reach patients when in-person meetings are not an option. These alternatives have supported some progress, but require access to high speed internet. Some rural areas are still underserved, particularly in Appalachia, where the technology and data plans necessary for telehealth can be hard to come by.
Taking Action
The severe increase in opioid overdoses and deaths seen during COVID-19 has caught the attention of the current administration. Addiction and overdoses were highlighted as a federal priority by the White House earlier this year. In March 2021, $4 billion was appropriated to the Substance Abuse and Mental Health Services Administration (SAMHSA) as part of the American Rescue Plan (ARP). The ARP also includes funding to expand access to broadband, especially in rural underserved areas, to support telehealth access and treatment.
To address issues related to accessing prescriptions for treatment, which can delay immediate care for OUD patients, HHS updated federal guidelines to expand the list of medical practitioners who can prescribe buprenorphine and other scheduled prescriptions. Tom Coderre, Acting Deputy Assistant Secretary for Mental Health and Substance Use at SAMHSA, stated in an HHS press release, “The spike we’ve seen in opioid involved deaths during the COVID-19 pandemic requires us to do all we can to make treatment more accessible.”
The CDC has also issued recommendations for addressing increasing deaths driven by synthetic opioids, including increased education and training for public health officials, health providers, and community organizations, and improving detection of dangerous substances such as fentanyl. (For more information on fentanyl and other substances, see our fact sheets, linked below under “additional resources.”)
Finally, federal oversight by agencies like the FDA, DEA, and CDC is essential for monitoring and reporting data on the prevalence of pain, the prescription of opioid analgesics, and the supply of illicit drugs; robust data can drive policies to address the opioid epidemic from different angles. An article published in the Journal of Health Politics, Policy, and Law recommended several policies and practices that can be adopted to combat the epidemic, such as expanding evidence-based addiction care through federal healthcare programs, improving pain treatments and access, and reducing exposure to drugs.
As the nation continues to combat COVID-19, health and policy leaders need to be nimble and responsive in finding ways to better provide services and treatments for patients with opioid use disorder. Continued research efforts such as the HEAL Initiative at NIH to provide funding for pain management research and the development of new strategies and therapies to treat OUD, pain, and overdose are vital in the continued battle against OUD.
Additional resources:
-
If you or anyone you know is seeking help for substance use disorder, please visit SAMHSA for a list of resources.
-
Share your concerns with your elected officials. The AMA has a list of actions states can take to curb opioid use disorder and overdoses.
-
Staying informed is a powerful way to continue the discussion on opioids. We have three fact sheets you can learn from, share with elected officials, and include in your communications.
Sophia Kaska, Ph.D. is the Manager of Science Initiatives and Outreach at Research!America with expertise in opioid pharmacology and addiction.
This article and accompanying fact sheet were made possible by the contributions of our current and past Science Policy Fellows Victoria Schneider, Ph.D., and Jessica Scott, Ph.D.; current and past Science Policy Interns Catherine Murphy and Ashni Dhruva; and current and past Science Communication Interns Caterina DiBiase and Samantha Mensah.




