Alliance Discussion with Dr. Abraham Verghese: The Art and Science of Human Connection
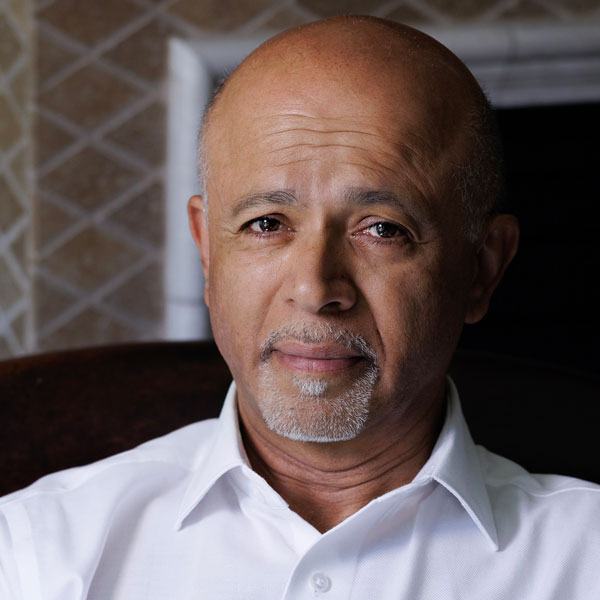
Dr. Abraham Verghese, Bestselling Author of Cutting for Stone and The Covenant of Water, and Linda R. Meier and Joan F. Lane Provostial Professor and Vice Chair of the Department of Medicine at Stanford University School of Medicine, joined us to discuss how his career in medicine and writing has shaped his outlook on the art and science of human connection. Here are some of his thoughts on:
The art and science of human connection in medicine:
“Medicine is ultimately a very human experience. As much as we can reduce physiology and organ systems to very orderly schematics, the essence of a human being ill is a very personal thing, and each person responds in a particularly unique way. William Osler famously said, “It is much more important to know what sort of patient has a disease than what sort of disease a patient has.” So, I think the essential art of being a physician, and the appealing part of it, to me, has been that we’re dealing with very different individuals who handle disease and stress very differently. We can plug a lot of things into artificial intelligence (AI), but not this. I always like the analogy of a newborn baby. We have the technology to care for a newborn child with robots if we ever decided to, but we would never dream of that, because they need the nurturing, they need parents to be involved. In the same way, I think there is something about illness, especially when it’s serious, that is fundamentally reducing you to a very elemental state, where whatever care you’re going to receive has to be delivered in the form of a caring person, the caring health care system, the caring society. That’s what makes this very much an art and a science.”
Incorporating research into storytelling:
“One of the great joys of being a physician, as long as I’ve been a physician, which is now almost 40 years, is in my lifetime watching things that we only had vague descriptors of, such as HIV, the years we spent not even knowing what it was, then we find the cause, then we understand the molecular mechanism, then, at some point, we sometimes a cure. Watching the evolution of medicine in my lifetime was one of the most exciting things that has happened. So, I deliberately wanted to have a novel that involves several generations. In the scope of the novel, you could see medicine evolve. And watching those three generations sort out what this was, was to me, part of the interesting thing about trying to write it and I think it captures what [Research!America] is about. What makes medicine so exciting is that without the research, without the advocacy, we’d be just dealing with the same diseases in the same way for decades. I think that’s what makes this so interesting.”
Involving patients in conceptualizing research programs:
“I think very often the heart of translational medicine is that a clinician identifies a problem, or a public member brings to light a problem. Then the translational part is trying to find the science and the research to solve that problem. So, I think it’s historically been huge groups of patients advocating for particular diseases; think of muscular dystrophy and MS. It’s always been there, I think. Engaging [patients] more formally at the granular individual lab level is an interesting idea.”
How to incorporate empathy, emotions, and storytelling into careers in STEM:
“I think that ‘story’ is inherent to science and medicine, though we may not always be conscious of it. Think of when you see a patient – you get a history. Well, the word ‘story’ is embedded in the word history. I think in retrospect, much of science winds up being compelling stories. It is helpful, I think, for anyone, not just scientists, to understand the nature of story. From the time of Aristotle, we’ve understood that the story is conflict, crisis, and resolution. To me, the importance of that is, as I like to tell my students in residence, even if something is routine for you, with a patient coming to see you, it has all the elements of conflict-crisis resolution, in the sense that every visit to a physician has the potential for some bad news coming around, some change in the trajectory. In Hollywood, they say drama equals desire plus danger where, you want something – desire, there’s some obstacle in the way – drama. You come to the doctor’s office with the desire to walk out of there, being told everything’s fine. In science, in pure research, I think that there are equally compelling stories, even if they’re happening at the molecular level. The challenge is to make that story translatable to people that don’t have the vernacular, that don’t have the applied vocabulary.”
Utilizing AI to ensure physicians maintain a human connection with their patients:
“The human connection between the physician and the patient is already very challenged, especially when you have large health care systems, merging venture capital firms buying systems and asking for a kind of productivity that is more typical of a car manufacturing factory. With so much turnover, so many different shifts, it’s a challenge to maintain that human connection. I think AI has a great potential to take away some of the drudgery in physicians’ lives. Right now, we are literally the highest paid clerical workers in the hospital, spending more time charting things than seeing patients. Every other time saving device has only meant more work for physicians and even less time to spend with the patient. My hope is that AI makes all the nuisance things for patients and physicians easier – checking in, checking out, filling out the same form 50 times. But I think it needs policing. It is neither artificial nor intelligent. It’s not artificial in the sense that it’s based on my work, your work, parasitizing everything we’ve ever written. It’s not intelligent enough to recognize human needs except in algorithmic fashion. The obstacle may not be computing power, it may be a willingness in Congress and the legislature to enact something so that we’re not a healthcare system based so much on fee-for-service that prioritizes procedures over dealing one-on-one with human beings.”
Dr. Verghese is the 2024 Advocacy Award recipient for the Isadore Rosenfeld Award for Impact on Public Opinion, an award presented annually to a news media representative or other influential individual who has been extraordinarily effective in delivering medical, public health, or other health-related research advocacy messages to the public. Register for this year’s Advocacy Awards and learn more about the 2024 honorees.




